In the rapidly evolving landscape of healthcare technology, few topics are as compelling—or as financially opaque—as Artificial Intelligence (AI). Hospital CTOs and MedTech founders recognize the transformative potential of an AI solution that can automate clinical workflows, improve diagnostics, or personalize treatment. Yet the question that halts most innovation projects is stark and simple: What is the real cost of developing medical AI software?
This uncertainty often serves as the biggest barrier to adoption, far outweighing the technical challenges. For a clinical-grade solution, the initial development investment alone typically ranges from $400,000 to $3,000,000, and that figure doesn't account for long-term compliance and maintenance costs. To dispel the myth of the "black box budget," we must move beyond simple project estimates and establish a granular, phase-by-phase cost model.
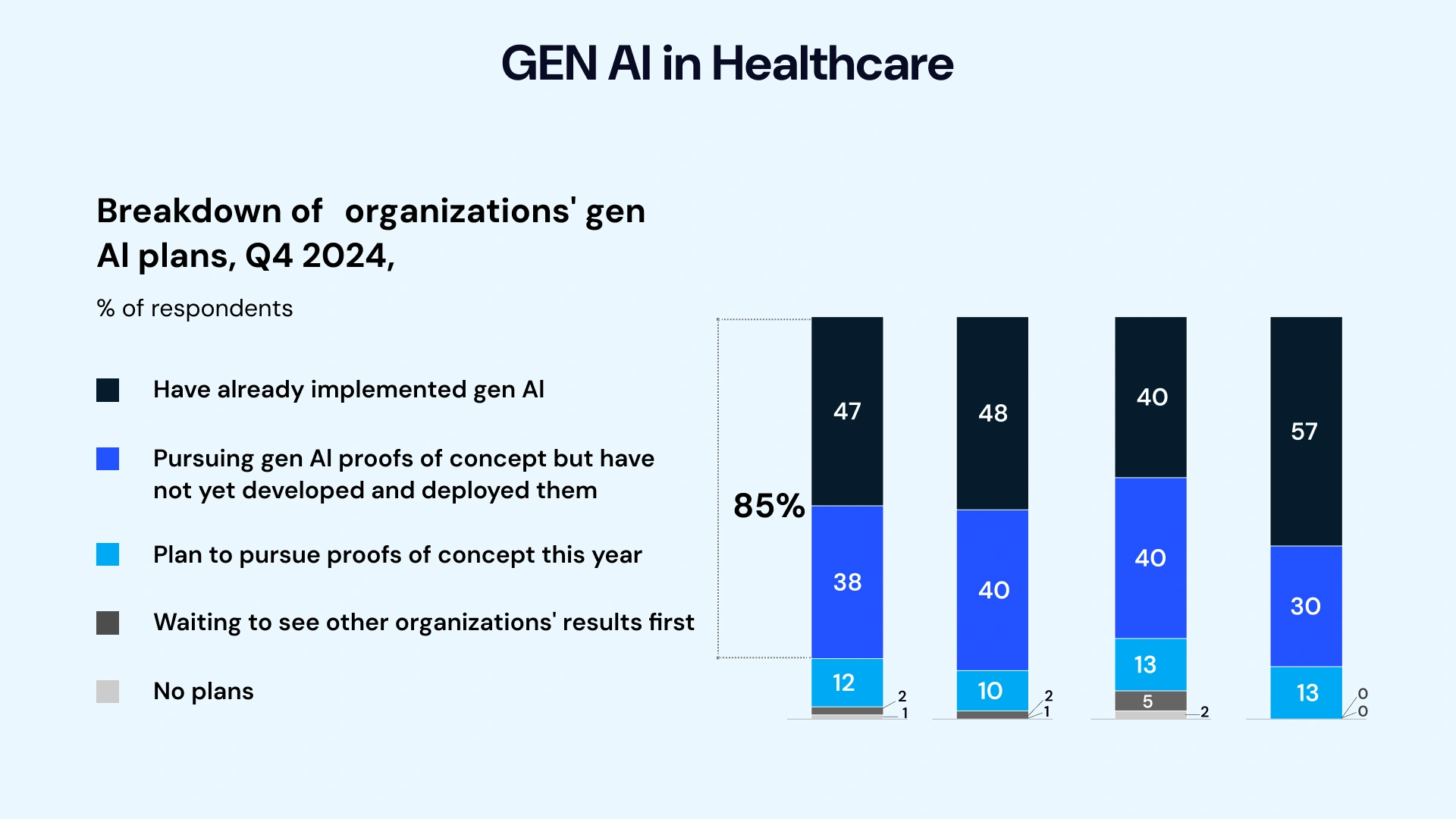
This seismic shift validates that the investment risk is no longer in whether to adopt AI, but in how to build the right, compliant solution efficiently.
For technology decision-makers, this guide is designed as your blueprint. Drawing on over a decade of experience building and validating clinical technology, we will break down the true total cost of ownership (TCO), from initial compliance audits to long-term model maintenance. You will get granular budget planning for developing medical AI software to build a compelling business case, select the right partners, and minimize the fear of project scope creep.
Understanding the Medical AI Software Landscape
The final cost to develop medical AI software is fundamentally determined by its complexity, the type of data it consumes, and its regulatory risk classification. A simple administrative tool will never command the same budget as an FDA-cleared diagnostic system.
Types of Medical AI Applications
Medical AI solutions fall into distinct categories, each with varying machine learning development costs for healthcare requirements:
- Diagnostic AI: Solutions like medical imaging analysis (radiology, pathology) or AI-powered EKG interpreters. These are high-risk, requiring massive, annotated datasets and stringent FDA clearance, leading to the highest development costs.
- Predictive AI (Prognostic): Tools that use structured and unstructured EHR data to predict patient outcomes (e.g., risk of sepsis, hospital readmission, or drug non-adherence). They require complex data integration and robust statistical validation.
- Generative AI: Focuses on content creation, such as clinical documentation (summarizing patient-physician encounters), drafting prior authorization requests, or personalizing patient communication. This segment is growing rapidly and can significantly reduce administrative overhead.
- Monitoring & Behavioral Health AI: This category, often underserved in general tech discussions, includes AI-powered mental wellness apps, remote patient monitoring (RPM) tools for chronic conditions, and AI chatbots for therapy support. They rely heavily on Natural Language Processing (NLP) and speech/sentiment analysis, requiring highly specialized, privacy-preserving datasets.
Regulatory Considerations: The Cost of Compliance
For any clinical-grade AI, compliance is not an optional feature; it’s a foundational cost driver. The difference between a simple, non-regulated wellness app and a regulated Medical Device Software (SaMD) often comes down to a six-figure regulatory budget.
- HIPAA & GDPR: Compliance with the U.S. The Health Insurance Portability and Accountability Act (HIPAA) and the European General Data Protection Regulation (GDPR) mandate strict, encrypted data handling, secure cloud infrastructure, and detailed audit trails. This increases the cost of the Custom medical AI solution for backend engineering and infrastructure.
- FDA Regulations (SaMD): The U.S. Food and Drug Administration (FDA) classifies AI tools based on their impact on clinical decisions. A system providing information to a doctor (Class I/II, often 510(k) pathway) is far less expensive to validate than one that drives autonomous treatment (Class III). The path to FDA clearance dictates the scope of clinical trials and the number of highly paid clinical specialists required for validation, thereby directly inflating the cost of building an AI diagnostic system.
| Regulatory Factor | Complexity Driver | Estimated Cost Impact (Per Phase) |
| HIPAA Compliance | Data infrastructure, encryption, access control (role-based), and legal audit. | $15,000 – $40,000 (Upfront setup) |
| FDA Class II (510(k)) | Clinical validation, documentation (e.g., Design History File), submission fees. | $100,000 – $500,000+ (Post-Model Development) |
| Data De-identification | Engineering time, specialized software, legal oversight. | $20,000 – $50,000 (Data Phase) |
Core Cost Components Breakdown: The Six Development Phases
To truly understand the cost of developing medical AI software, we must itemize the expenses across the full lifecycle. A typical AI development services project can be broken down into six critical phases.
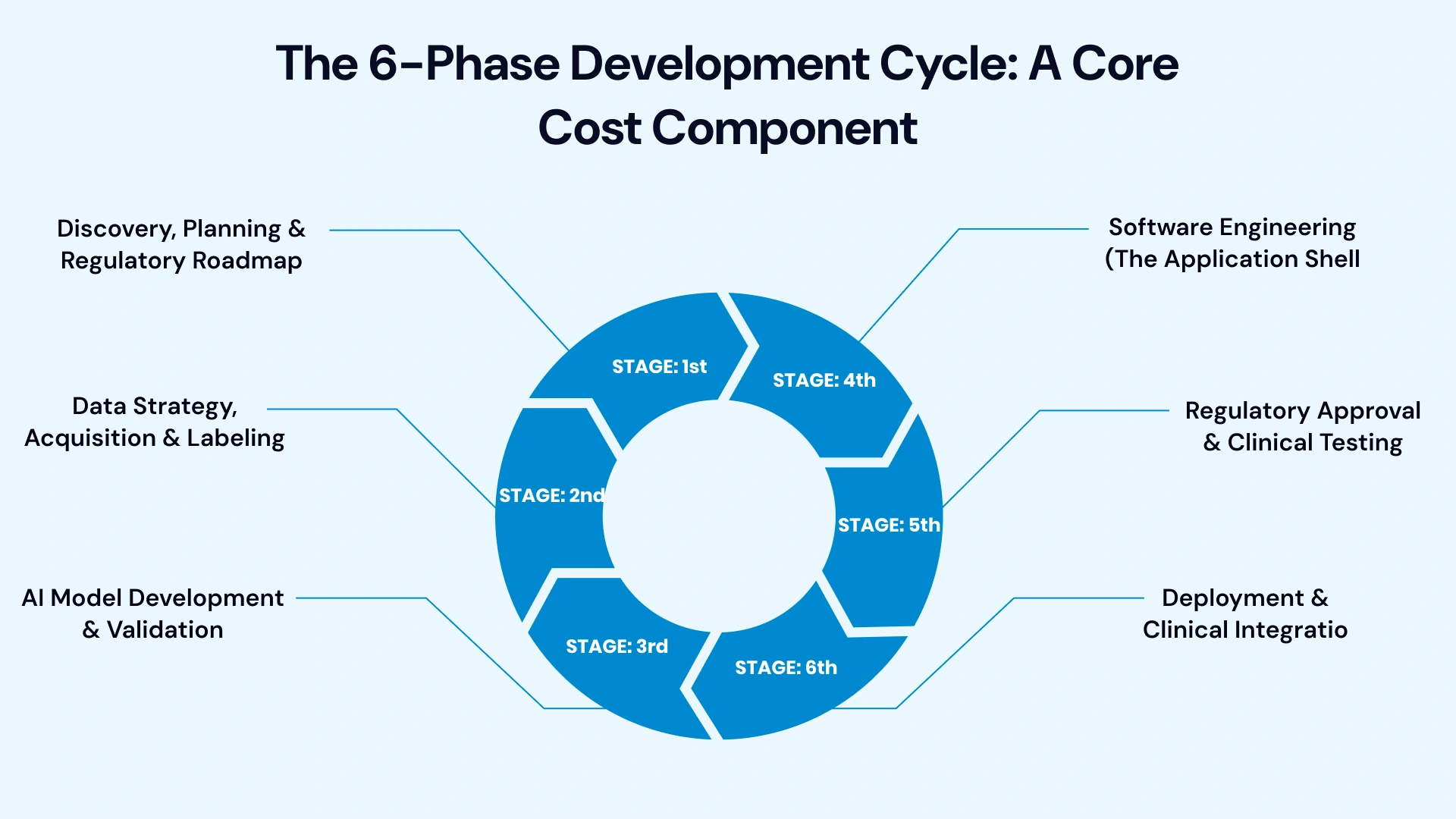
Phase 1: Discovery, Planning & Regulatory Roadmap
This phase is the cheapest but arguably the most crucial for mitigating later scope creep and for determining the full budget for developing medical AI software.
- Key Deliverables: Detailed requirements (PRD), Technical Architecture Blueprint, Regulatory Strategy Document, Feasibility Study, MVP Scope Definition.
- Key Personnel: Business Analyst, Solution Architect, Regulatory Counsel/Consultant.
- Cost Drivers: Clarity of the problem statement, complexity of existing system integration (EHR/PACS).
- Cost & Timeframe:
- Time: 4–8 Weeks
- Cost Range: $25,000 – $75,000 (A critical investment to avoid millions in sunk costs later).
Phase 2: Data Strategy, Acquisition & Labeling
AI is only as good as its data. In healthcare, data is scarce, siloed, and often unstructured. This phase defines the difference between a functional product and a clinically valid one.
- Key Deliverables: Data Acquisition Plan, Labeled Dataset, Data Privacy Policy (DPA/BAA), Data Storage Infrastructure (HIPAA-compliant cloud).
- Key Personnel: Data Scientist, Data Engineer, Clinical Domain Expert (for labeling).
- Cost Drivers:
- Dataset Acquisition: Purchasing large, diverse, pre-labeled datasets (e.g., radiology images) can cost $20,000 or more.
- Data Labeling Cost for Medical Datasets: This is a hidden expense. For computer vision or complex NLP, human experts (e.g., board-certified radiologists or licensed therapists) must annotate data. Simple labeling may cost $1–$5 per instance, but complex clinical annotation can cost $10–$50 per instance, often totaling $50,000-$250,000 for a robust dataset.
- Cost & Timeframe:
- Time: 2–6 Months
- Cost Range: $75,000 – $350,000+
Phase 3: AI Model Development & Validation
This is the core engineering effort where the system's "smarts" are built. The Machine learning development cost for healthcare hinges on whether you use pre-trained models or create a custom solution.
- Key Deliverables: Trained and Validated Model, Training/Testing Pipeline, Model Performance Report (AUC, F1 Score, Sensitivity/Specificity).
- Key Personnel: Machine Learning Engineer, Data Scientist, MLOps Engineer.
- Cost Drivers:
- Algorithm Complexity: Deep Learning (e.g., Computer Vision for pathology) is more complex and requires more compute than simpler, classic ML models (e.g., Random Forest for predictive analytics).
- Compute: Cloud-based GPU training can be costly. For large foundation models, training runs can cost $10,000 to $ 50,000 or more in cloud services alone.
- Custom vs. Transfer Learning: Building a custom model from scratch is highly resource-intensive. Fine-tuning an existing, pre-trained model (Transfer Learning) significantly reduces the AI development timeline and cost.
- Cost & Timeframe:
- Time: 3–9 Months
- Cost Range: $90,000 – $400,000+
Phase 4: Software Engineering (The Application Shell)
The model needs a user interface, a secure backend, and integration capabilities to be clinically helpful. This is where the Custom medical AI solution cost for UX, backend, and security is realized.
- Key Deliverables: Front-end Application (Web/Mobile), Secure API, EHR Integration Modules (e.g., FHIR-compliant interfaces), System Security Audit.
- Key Personnel: Full Stack Developers, DevOps Engineer, UI/UX Designer.
- Cost Drivers:
- Integration Complexity: Deep, bi-directional integration with multiple EHR systems (Epic, Cerner) is notoriously time-consuming and expensive, often adding $30,000 to $150,000 per integration.
- User Interface: Clinical UX must prioritize speed and clarity, which requires specialized design and rigorous user testing with clinical staff.
- Cost & Timeframe:
- Time: 4–8 Months (often running in parallel with Phase 3)
- Cost Range: $100,000 – $300,000
Phase 5: Regulatory Approval & Clinical Testing
This is the make-or-break phase for any Class II or Class III medical device software development. This cost is a non-negotiable part of implementing AI in healthcare for a clinical setting.
- Key Deliverables: Finalized Design History File (DHF), Clinical Trial/Retrospective Study Report, FDA/CE Submission Package, QMS (Quality Management System) Audit.
- Key Personnel: Regulatory Affairs Specialist, Clinical Research Coordinator, Biostatistician.
- Cost Drivers:
- Clinical Validation: The scale and duration of the clinical study are required to prove safety and efficacy. A small retrospective study costs significantly less than a multi-site prospective trial.
- Submission Fees: FDA fees are variable but make up only a small part of the total cost; the bulk of the price is labor for documentation.
- Cost & Timeframe:
- Time: 6–18 Months
- Cost Range: $150,000 – $1,000,000+ (Highly dependent on risk class and trial scope).
Phase 6: Deployment & Clinical Integration
The final step is moving from the sandbox to the live environment, often involving on-premise or hybrid cloud costs for AI model deployment.
- Key Deliverables: Production Environment Setup, IT Security Sign-off, Staff Training Materials, Go-Live Plan.
- Key Personnel: DevOps Engineer, IT Security Officer, Implementation Specialist.
- Cost Drivers:
- On-prem vs. Cloud AI Pricing: Hospitals with legacy systems may prefer on-prem installation, which carries high upfront hardware costs (servers, GPUs: $50,000+) but lower operational costs over time. Cloud deployment (AWS, Azure, GCP) has lower upfront costs but higher monthly cloud costs for AI model deployment, based on usage.
- Cost & Timeframe:
- Time: 1–3 Months
- Cost Range: $30,000 – $120,000 (Plus ongoing cloud/maintenance costs).
Real-World Cost Scenarios: Itemized Budgets
The true cost of developing medical AI software is best illustrated by looking at three distinct use cases, from the low-to-medium complexity of a mental health chatbot to the high-stakes complexity of a diagnostic tool.
Scenario A: AI Mental Health Chatbot (Low-Medium Complexity)
- Use Case: An AI-enabled chatbot for a Behavioral Health Provider network that screens patients for anxiety/depression using conversational NLP and provides HIPAA-compliant psychoeducational resources.
| Phase | Key Activities | Estimated Cost Range (USD) |
| 1: Discovery | Requirements, NLP selection, HIPAA compliance roadmap | $25,000 – $35,000 |
| 2: Data Strategy | Acquiring labeled dialogue data, de-identification, and custom sentiment labeling | $40,000 – $80,000 |
| 3: Model Dev | Fine-tuning a ClinicalBERT model for sentiment, toxicity detection, and validation | $80,000 – $150,000 |
| 4: Software | Mobile app/Web interface, secure backend, EMR API integration (light) | $120,000 – $200,000 |
| 5: Regulatory | Legal review (HIPAA/GDPR), QMS setup, non-FDA clearance pathway (low-risk) | $30,000 – $75,000 |
| 6: Deployment | Cloud setup (minimal compute), staff training | $25,000 – $40,000 |
| Total Estimated Cost of Developing Medical AI Software (MVP): | $320,000 – $580,000 |
Scenario B: AI Diagnostic Imaging Tool (High Complexity)
- Use Case: A deep learning model that analyzes chest X-rays (DICOM images) in real-time to flag urgent conditions like pneumothorax, acting as a Class II SaMD.
| Phase | Key Activities | Estimated Cost Range (USD) |
| 1: Discovery | Clinical workflow analysis, DICOM standard integration plan | $40,000 – $80,000 |
| 2: Data Strategy | Data Labeling Cost for Medical Datasets (radiologist annotation of 100k images), PACS integration, HIPAA compliance | $200,000 – $450,000 |
| 3: Model Dev | Custom CNN development, large-scale GPU training, rigorous cross-validation | $350,000 – $800,000 |
| 4: Software | PACS integration, real-time alerting system, enterprise dashboard | $180,000 – $350,000 |
| 5: Regulatory | Clinical trial management (retrospective or prospective), DHF, FDA 510(k) submission, and labor (the core AI system validation cost (healthcare)) | $300,000 – $1,000,000 |
| 6: Deployment | On-premise server setup (GPU purchase), hospital IT integration | $100,000 – $250,000 |
| Total Estimated Cost to Build AI Diagnostic System (V1.0): | $1,170,000 – $2,930,000+ |
Scenario C: Predictive Analytics Dashboard (Medium Complexity)
- Use Case: A predictive risk model for health systems to identify patients with a high probability of 30-day readmission using structured and unstructured EHR data.
| Phase | Key Activities | Estimated Cost Range (USD) |
| 1: Discovery | Risk factor identification, clinician interviews, ROI modeling | $30,000 – $50,000 |
| 2: Data Strategy | Multi-source EHR data extraction/cleaning, feature engineering, data quality audits | $100,000 – $200,000 |
| 3: Model Dev | Developing a multi-factor ML model, explainability module (XAI) | $150,000 – $280,000 |
| 4: Software | Interactive dashboard/interface, API for EMR population health module | $100,000 – $180,000 |
| 5: Regulatory | Internal validation of model fairness/bias, legal compliance check (non-clinical device) | $20,000 – $40,000 |
| 6: Deployment | Cloud-based serverless deployment, integration with existing IT infrastructure | $40,000 – $70,000 |
| Total Estimated Cost of Implementing AI in Healthcare (V1.0): | $440,000 – $820,000 |
Hidden Costs and Long-Term Considerations: The AI TCO
The initial development cost is just the down payment. Savvy CTOs and Digital Health VPs must consider the Total Cost of Ownership (AI TCO (total cost of ownership) healthcare) to calculate the eventual ROI accurately. These recurring expenses are where projects often fail to meet long-term budget projections.
1. Ongoing Model Retraining and Maintenance
AI models degrade over time. Clinical protocols change, patient populations shift, and a model’s accuracy can drift—a phenomenon known as model decay.
- Cost of Maintenance for Medical AI Tools: This is a continuous operational cost. Expect to allocate 20% to 35% of the initial development cost annually for MLOps, model monitoring, and retraining runs to maintain clinical efficacy.
- Compliance Updates: When the FDA updates its guidance on SaMD (e.g., changes to Real-World Performance monitoring), your internal systems and documentation must be updated, incurring specialized engineering and regulatory labor.
2. Cloud and Compute Costs
For scalable solutions, your monthly bill from AWS, Azure, or Google Cloud is a critical factor.
- Cloud Cost for AI Model Deployment: This covers storage, compute (inference), and networking. A large-scale diagnostic AI analyzing millions of images per month can easily incur monthly cloud costs of $5,000 to $20,000+.
- Data Storage and Archiving: Healthcare data must often be archived for decades for regulatory and legal reasons, requiring massive, long-term, HIPAA-compliant storage, which is expensive at scale.
3. Talent Acquisition and Insurance
Building an AI solution requires not just developers but highly specialized, highly paid personnel.
- Talent: Maintaining an in-house MLOps team means salaries for Data Scientists and ML Engineers, which average well over $150,000 in major tech hubs. This is the argument for outsourcing to reduce the AI consulting cost in healthcare.
- Insurance: A critical, often-overlooked cost is increased liability insurance coverage. If your AI is used to make a diagnostic or treatment recommendation (SaMD), your malpractice insurance premiums will rise, requiring careful risk assessment with legal counsel.
Cost Optimization Strategies: Reducing the Total Investment
The financial barrier to entry is high, but strategic planning can significantly reduce the cost of implementing AI in healthcare without sacrificing clinical quality.
1. Build vs. Buy: When to Leverage Pre-Trained Models
The single biggest factor in the initial cost of the Custom medical AI solution is the decision to build from scratch.
- Build: Custom software development is essential for niche problems, proprietary data sets, and competitive differentiation (e.g., an AI for a rare disease). This pathway is expensive and requires a long AI development timeline.
- Buy/Fine-Tune: For common tasks (e.g., general NLP, basic image classification), leverage existing foundational models (e.g., BioBERT, ClinicalGPT, pre-trained image encoders). This drastically reduces training time and associated compute costs, lowering the initial investment by up to 50%.
2. Prioritize a Focused Medical AI MVP Development Cost
Avoid feature creep. The goal of aMinimum Viable Product (MVP) in healthcare is not just to launch quickly, but to achieve clinical validation as soon as possible.
- Start with a Narrow Scope: Focus the MVP on a single, high-ROI workflow (e.g., flagging only one high-risk condition, not ten).
- Phased Rollout: Deploy in one clinical department or hospital first, then use that validated success to secure the budget for full-scale launch. This mitigates the risk of a massive failure and enables early ROI to fund the next phase.
3. Partner with Specialized AI Development Firms
Engaging a partner with deep, pre-existing knowledge of the regulatory and clinical technology stack reduces the need for expensive, long-term in-house hiring.
- Expertise in Compliance: A specialized partner offers a ready-made Quality Management System (QMS) and streamlined documentation processes, drastically reducing time and labor costs in Phase 5 (Regulatory).
- Efficiency: They often have pre-built codebases for EHR integration and HIPAA compliance, directly reducing your cost of developing medical AI software for the software engineering phase.
ROI and Value Realization Timeline in Healthcare AI
The return on investment (ROI) in healthcare AI is generally measured not just in dollars but in clinical and operational efficiencies.
Key Metrics for Measuring AI Success in Healthcare
- Clinical: Reduction in False Negatives (FN) and False Positives (FP), improved diagnostic agreement (Kappa score), and time-to-treatment.
- Financial/Operational: Decrease in hospital readmission rates, reduction in administrative labor hours (cost savings from AI automation in hospitals), and faster turnaround time for procedures.
Expected Payback Periods
While highly variable, the payback period for healthcare AI tends to follow the complexity curve:
| AI Solution Complexity | Primary Value Driver | Expected Payback Period |
| Low (Admin Automation) | Labor cost reduction, increased throughput | 6–12 Months |
| Medium (Predictive Analytics) | Reduced adverse events (readmissions, risk events) | 12–24 Months |
| High (Diagnostic SaMD) | New revenue stream, improved patient outcomes, competitive advantage | 24–48 Months (Post-FDA Clearance) |
The economic benefits of medical AI software are clear: automating documentation with generative AI can save a physician 1-2 hours per day, translating into hundreds of thousands of dollars in saved salaries and increased patient throughput annually. This is the long-term value that justifies the high upfront cost to develop medical AI software.
Future of Medical AI Software
The current era of medical AI is primarily focused on assistive AI—tools that help clinicians read images faster or draft patient notes. The next five years will usher in a critical transition where the focus shifts to Autonomous AI Agents, Hyper-Personalization, and the pervasive adoption of Generative AI Copilots, fundamentally changing the development cost landscape.
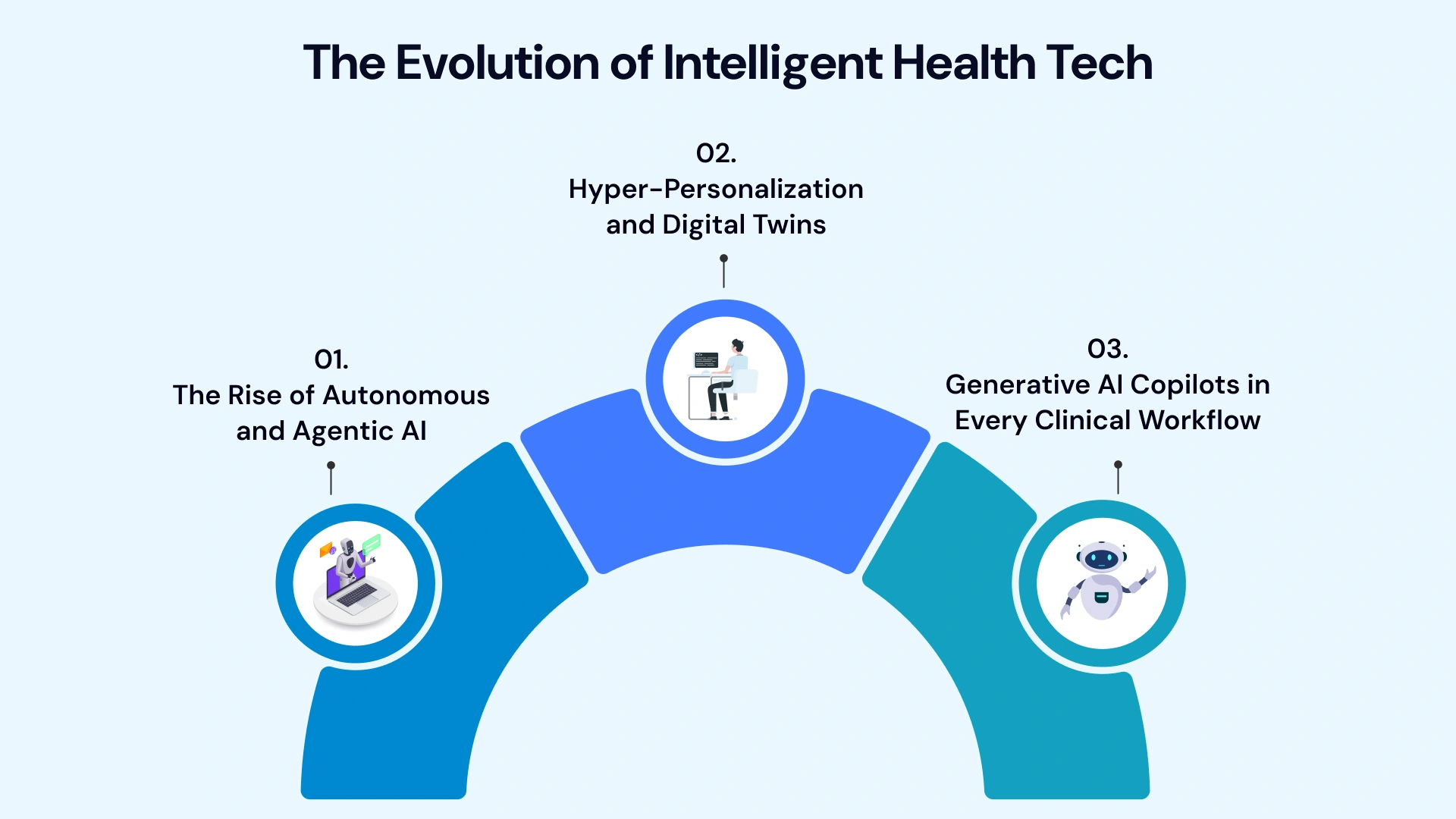
1. The Rise of Autonomous and Agentic AI
The evolution is moving from tools that offer insights to agents that execute complex, multi-step tasks independently.
- Agentic AI: These systems will be able to autonomously manage entire workflows, such as processing a lab result, checking it against a patient's EHR, generating a draft treatment adjustment, and queuing it for physician review. This dramatically increases the need for sophisticated MLOps, security controls, and fail-safe mechanisms, raising the cost of development (Phase 4) but delivering massive cost savings from AI automation in hospitals (ROI).
- Autonomous Diagnostics: The future will see more Class III SaMD tools cleared for autonomous diagnostic decisions in specific, tightly controlled environments, such as detecting critical findings on an X-ray without immediate human intervention. This will necessitate higher AI system validation costs (healthcare) due to the required rigor of clinical trials.
2. Hyper-Personalization and Digital Twins
The convergence of AI with massive genomic and real-time physiological data will make generalized medicine obsolete.
- Digital Twins: AI will power "digital twins" of individual patients or entire hospital systems. A patient's twin can simulate the effect of various chemotherapy regimens or surgical approaches before treatment is administered, allowing for optimal decision-making and reduced adverse events.
- Genomic AI: AI will integrate genomic data with clinical history, lifestyle factors, and environmental data to design precision drug delivery and dosing schedules, shifting the cost of developing medical AI software away from broad population-based studies toward highly specialized longitudinal data infrastructure (Phase 2). This is the key to unlocking the actual financial benefits of medical AI software through avoided ineffective treatments.
3. Generative AI Copilots in Every Clinical Workflow
Generative AI will move beyond simple clinical note-taking to become an embedded clinical assistant across all administrative and diagnostic touchpoints.
- LLMs for Clinical Decision Support (CDS): The best Large Language Models (LLMs) trained on proprietary, secure medical knowledge will serve as robust CDS systems. They will synthesize massive quantities of medical literature, patient records, and current guidelines to provide real-time, evidence-based assistance. This capability will be crucial for managing the exponential growth of medical knowledge.
- Impact on Cost: While the base models are becoming commoditized, the cost to develop medical AI software for these copilots is shifting to the creation of secure, clinically validated, retrieval-augmented generation (RAG) pipelines and complex integration with existing EHR systems (Phase 4), ensuring accuracy and preventing "hallucinations" in critical patient care.
Choose VLink Expertise to Develop Medical AI Software
Moving a medical AI concept to clinical reality requires a blend of cutting-edge machine learning and rigorous regulatory expertise. The decision to partner is often the most cost-effective path, allowing you to avoid the massive upfront investment required to build a specialized, in-house compliance and MLOps team.
VLink specializes in Healthcare Software Development Services, bringing deep experience in HIPAA and FDA SaMD pathways to ensure your solution is secure, scalable, and clinically trusted from day one.
Our six-phase methodology is designed to minimize your AI project estimate for medtech startups by prioritizing a clinical-grade MVP and leveraging pre-built, compliant EHR integration and data-handling frameworks. We reduce the AI development timeline and ensure your long-term maintenance costs for medical AI tools remain predictable—partner with our dedicated team to transform your vision into a responsible, high-ROI AI solution.
Conclusion
The journey from a whiteboard concept to a clinically validated medical AI tool is lengthy, complex, and certainly not cheap. Whether you’re a Hospital CTO seeking the cost of implementing AI in healthcare to streamline operations or a MedTech Founder defining your initial Medical AI MVP development cost, the challenge is managing the risk of the unknown.
The actual cost to develop medical AI software is not a fixed price, but a sum of strategic, compliance-driven decisions. The leaders who succeed will be those who treat the regulatory pathway as an integrated cost component, not an afterthought, and who focus their initial investment on granular data strategy and targeted MVP development. By using this detailed six-phase cost blueprint, you gain the transparency needed to move your project from budgetary uncertainty to a powerful, clinically validated solution.
Ready to transform your clinical operations with a cost-optimized, compliant AI solution? Contact us today to schedule a focused discovery session where we’ll build your customized, phase-by-phase development and compliance roadmap.








 Shivisha Patel
Shivisha Patel