AI for treatment personalization is rapidly transitioning from a technology concept to a non-negotiable financial imperative across North American healthcare. For hospitals, providers, and pharmaceutical firms in the US and Canada, the conversation is no longer about whether they should adopt artificial intelligence in personalized medicine, but how quickly they can realize a measurable Return on Investment (ROI) to secure a competitive edge.
In an industry facing unprecedented margin pressure and a mandatory shift to value-based healthcare enabled by AI, a strategic Cost-Benefit Analysis (CBA) is essential. This analysis breaks down the total investment required, quantifies the massive savings and revenue opportunities, and provides a clear framework for deploying AI for treatment personalization to drive both superior clinical outcomes and profound financial gains.
The Market Overview: The Unavoidable Economic Shift
The US Healthcare Software Development Services, currently spending an estimated 5-10% on avoidable costs, could save $200 billion to $360 billion annually by adopting AI more broadly. This massive potential for AI's economic impact in healthcare positions AI-driven treatment personalization as the single most critical investment to mitigate risk and capitalize on the future of precision medicine technology.
The top AI workloads in healthcare are currently data analytics (58%), Generative AI (54%), and Large Language Models (LLMs) (53%). The immediate impact of these tools is clear: workflow automation (48% for providers) and drug discovery and development (59% for pharma).
The successful integration of AI for treatment personalization rests on leveraging these foundational technologies to move beyond basic diagnostics and directly influence clinical management.
Decoding the Technology: The Mechanics of Predictive Care
Understanding the components of a functional AI treatment personalization platform is vital for accurate cost modeling and justifying the ROI of AI in personalized treatment. The personalized medicine paradigm is fueled by machine learning development services, which process vast, multimodal datasets.
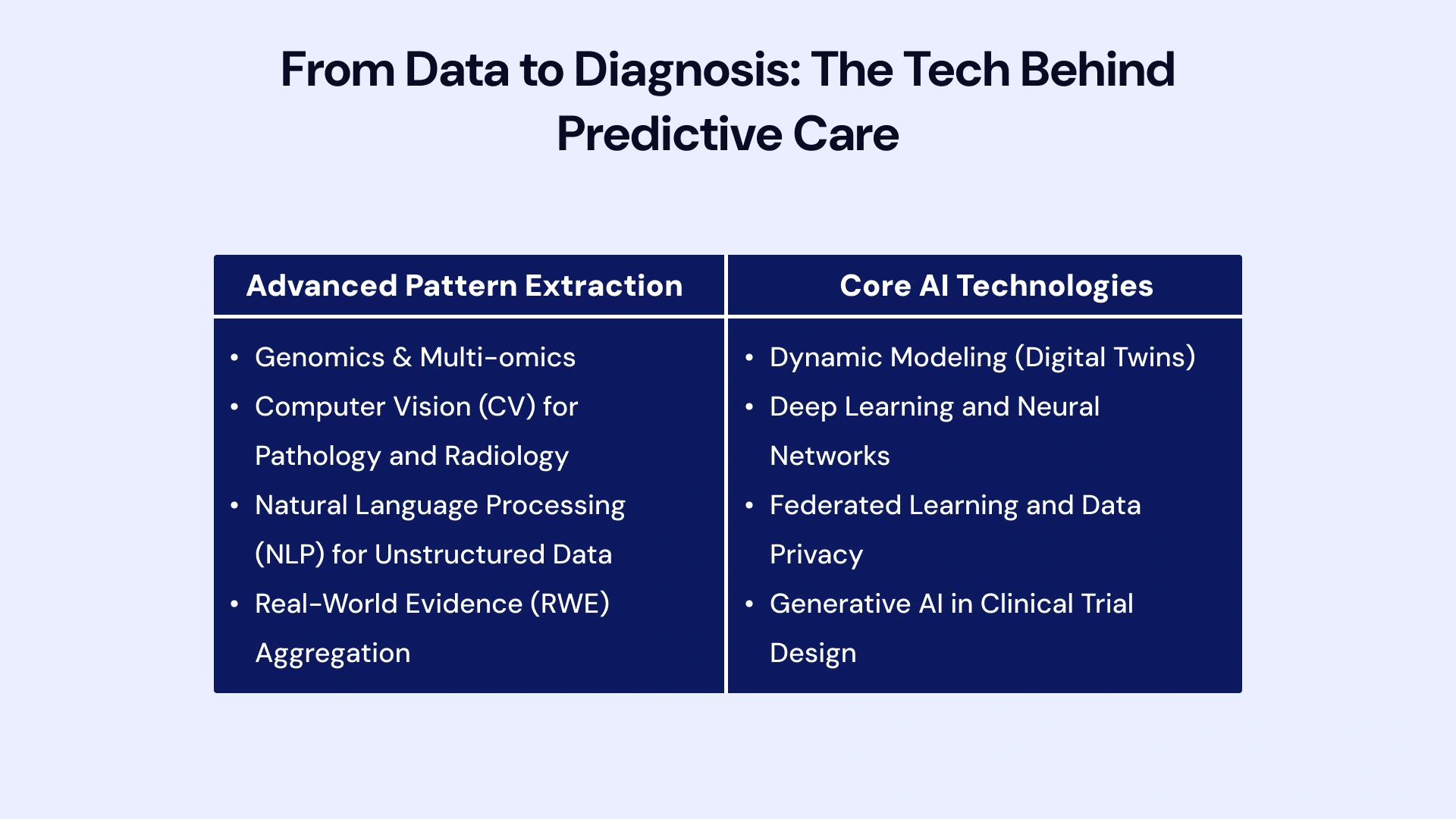
Advanced Pattern Extraction
AI systems analyze data points invisible to the human eye at scale:
- Genomics & Multi-omics: Identifying rare mutations or complex polygenic risk scores that dictate drug metabolism or disease progression. This requires specialized precision medicine technology to handle petabytes of sequencing data.
- Computer Vision (CV) for Pathology and Radiology: Applied in AI for radiology and imaging-based treatment guidance to segment tumors, predict response to radiation therapy, or detect subtle signs of disease progression in pathology slides—often flagging malignancy indicators far earlier than the human eye alone.
- Natural Language Processing (NLP) for Unstructured Data: Used to mine unstructured clinical narratives, discharge summaries, and historical treatment outcomes from the Electronic Health Record (EHR) to create a comprehensive patient profile for predictive analytics for patient outcomes. NLP tools extract crucial details, such as smoking status and severity modifiers, that are often missing from structured data fields.
- Real-World Evidence (RWE) Aggregation: Incorporating external data sources—claims data, pharmacy refill data, and patient-reported outcomes (PROs)—to build a full, longitudinal picture. The accuracy of the AI treatment personalization platform is directly proportional to the quality and breadth of this RWE.
Core AI Technologies at Play
- Dynamic Modeling (Digital Twins): Beyond static risk scores, advanced AI for treatment personalization uses algorithms to create virtual "digital twins" of individual patients, allowing clinicians to test the likely outcomes of different therapies (e.g., drug A vs. drug B) before administering them, providing crucial AI for clinical decision support.
- Deep Learning and Neural Networks: These techniques are paramount for processing complex, high-dimensional data, such as raw genomic sequences and images. They excel at AI-enabled risk stratification, clustering patients into highly specific, previously unrecognized subgroups that share a unique response profile to a treatment.
- Federated Learning and Data Privacy: Given the strict data regulations (HIPAA/PHIPA), future artificial intelligence in personalized medicine often relies on federated learning, where models are trained locally across multiple institutions, and only the weights (not the raw data) are shared. This enables powerful population-level learning without compromising patient privacy.
- Generative AI in Clinical Trial Design: Generative models are being used to simulate synthetic control arms for clinical trials and optimize protocols, thereby advancing AI for clinical practice optimization and reducing the overall cost of trial execution.
The Cost Equation: Deconstructing the Investment in Treatment AI
The TCO for AI for treatment personalization is substantial, requiring capital expenditure (CapEx) for acquisition and significant operational expenditure (OpEx) for maintenance, compliance, and continuous optimization. Ignoring these secondary costs is the primary reason why AI cost reduction in treatment personalization initiatives fails.
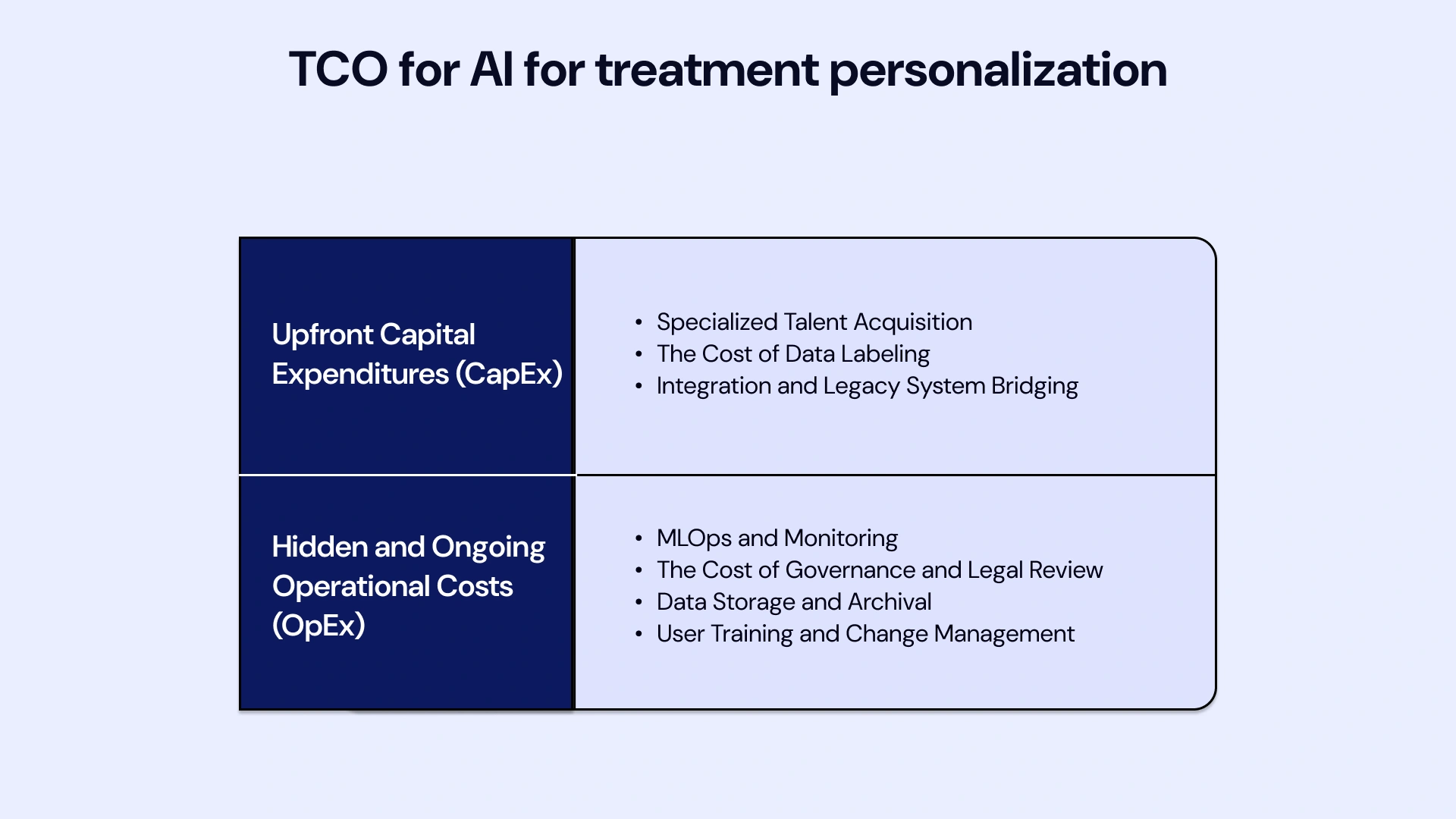
Upfront Capital Expenditures (CapEx)
Initial investment costs can range dramatically, often necessitating a detailed cost-benefit analysis of AI in healthcare before procurement.
- Specialized Talent Acquisition: The salary and relocation costs for specialized talent—ML engineers, clinical informaticists, and MLOps experts—are higher than for general IT staff. Building an in-house clinical AI model development services team can easily cost $1M+ in annual salaries alone.
- The Cost of Data Labeling: Data preparation is a heavy lift. High-quality model training for tasks like AI for oncology treatment planning requires thousands of expert-labeled images or charts. The cost of hiring specialized physicians or pathologists to label this data, often outsourced, can be $50,000 to $200,000 per model.
- Integration and Legacy System Bridging: Utilizing Healthcare Software Development Services to successfully integrate the new AI for personalized patient management tool with aging or proprietary EHR systems is complex. This often involves building custom wrappers and APIs to ensure data flows securely and in real-time.
Hidden and Ongoing Operational Costs (OpEx)
Sustainability relies on managing recurring costs, which are often underestimated in the initial budget.
- MLOps and Monitoring (The Hidden Cost): Maintaining models in production (MLOps) includes continuous re-training (model refresh) and drift monitoring. For complex models, the annual maintenance fee can range from 15% to 25% of the initial CapEx, covering the specialized teams required to ensure the AI for personalized patient care remains accurate.
- The Cost of Governance and Legal Review: Before a new model can touch a patient, it requires extensive internal legal and ethical review to confirm non-bias and explainability. The legal costs associated with obtaining approvals for AI in personalized medicine within the US (FDA) and Canadian (Health Canada) frameworks add significant recurring administrative overhead.
- Data Storage and Archival: Storing massive datasets required for AI-driven personalized treatment plans—mainly longitudinal genomic and imaging data—can lead to unexpectedly high cloud storage fees that grow by 30-50% annually.
- User Training and Change Management: The investment in training clinicians to trust and correctly interpret AI for clinical decision support is essential. Failure to invest in change management leads to poor adoption, rendering the entire CapEx investment worthless.
Central Analysis: The Cost-Benefit Framework for AI Personalization
The CBA must use advanced economic metrics to capture the value of AI for treatment personalization accurately. The average return of $3.20 for every $1 invested is a strong starting point, but granular analysis is needed to secure executive buy-in.
Quantifying the Clinical ROI: Outcomes as Financial Gains
Clinical improvement directly reduces the high costs of failure and complications, thereby improving the affordability of AI-driven personalized medicine.
- Net Present Value (NPV) and Cost-Benefit Ratio (CBR): Financial leadership requires calculating the NPV over a 5-10-year period, accounting for the discount rate. A successful AI implementation should aim for a CBR greater than 1.5 to demonstrate superior return compared to traditional IT investments.
- Specific Complication Avoidance: Quantify the financial impact of avoiding specific events. For example, using AI for precision dosing to prevent one severe Adverse Drug Event (ADE) in a high-risk patient can avoid an estimated $5,000 to $15,000 in complication treatment and extended LOS.
- Revenue from Increased Elective Capacity: By reducing LOS and avoiding readmissions, AI for hospital treatment optimization frees up high-demand beds. This allows the hospital to schedule more profitable elective surgeries or procedures, providing a direct revenue uplift.
Operational and Financial Efficiency
These benefits deliver rapid, bottom-line impact, fulfilling the need for AI-driven cost savings in patient care.
- Workforce Optimization and Retention: AI automates tedious data summarization, reducing burnout among physicians and nurses. The cost of replacing a physician is estimated at $250,000 to $500,000; AI’s role in retaining clinical talent is a significant, often overlooked, financial benefit.
- Supply Chain and Inventory Management: AI can predict the volume of specific treatments or drugs needed based on localized AI for population health personalization models, reducing inventory waste for high-cost, specialized therapeutics (e.g., targeted oncology drugs).
- Claims Denial Reduction: Predictive models can assess documentation completeness and accuracy before claims submission, significantly reducing claims denial rates and preventing costs of rework and lost revenue for health systems.
Strategic and Revenue Growth
The long-term value creation is realized through competitive advantage.
- Incremental Revenue from Specialized Services: The ability to offer highly specialized AI-driven precision treatments (such as specific gene therapies) attracts new patient populations and justifies higher service-line pricing, especially in cancer centers and specialized clinics.
- Research Grant Competitiveness: Demonstrating sophisticated use of AI for personalized patient management and AI for personalized therapy optimization enhances an institution’s competitiveness for major governmental and private research grants.
- Payer Contract Negotiation Leverage: Hospitals can use documented ROI from AI for early diagnosis and personalized interventions, and AI for personalized treatment plans to negotiate more favorable, outcome-based reimbursement contracts with private payers, directly impacting margin.
High-Value Use Cases: Proven ROI by Clinical Domain
Strategic investment requires prioritizing domains where the cost of failure is highest, and the data is richest, proving how AI improves treatment outcomes.
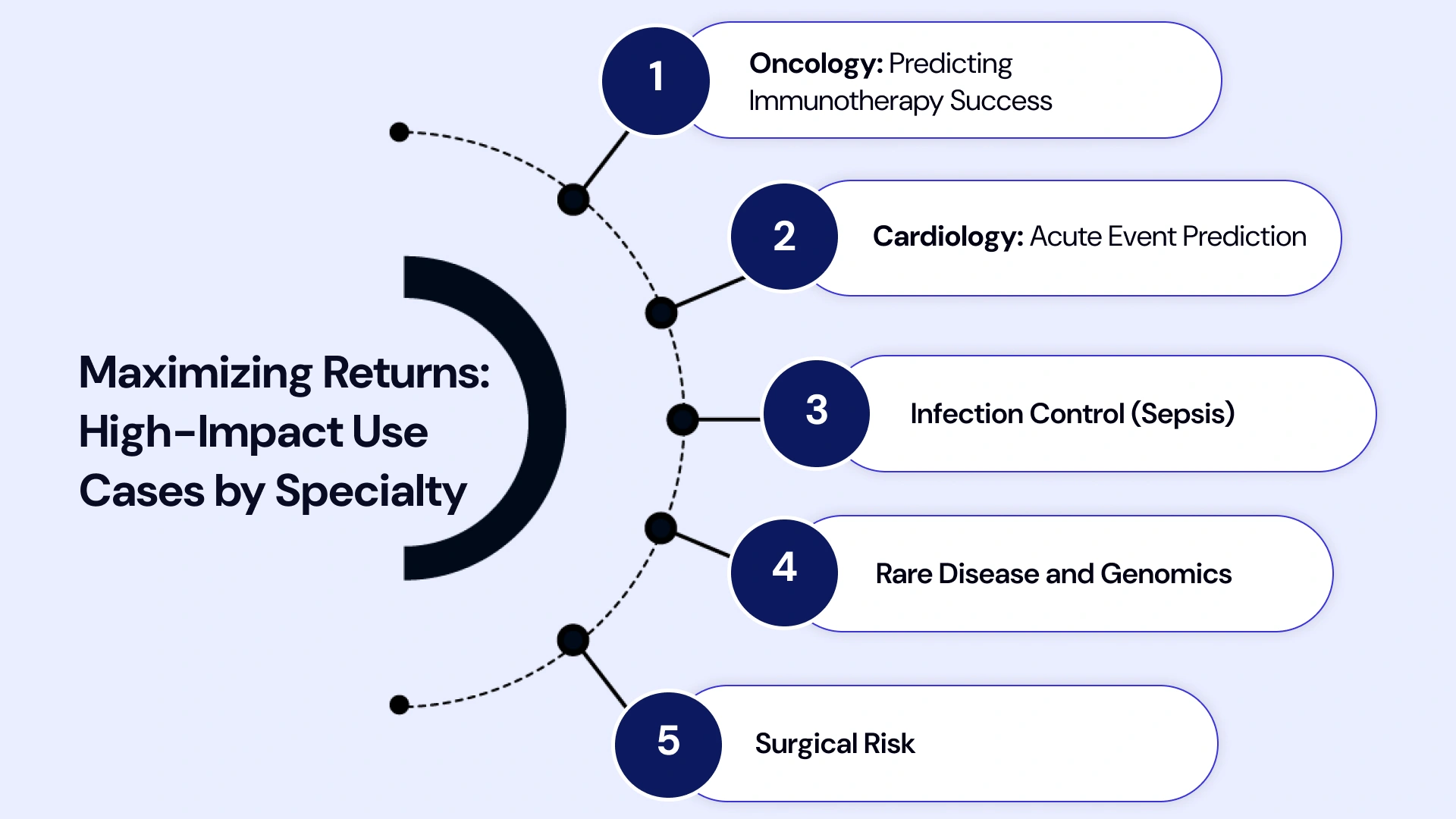
- Oncology: Predicting Immunotherapy Success: AI in precision oncology uses advanced genomic signatures (e.g., Tumor Mutational Burden) and imaging markers to predict which patients will respond to expensive immunotherapies rather than standard chemotherapy. This precision saves the system up to $150,000 per patient who avoids a futile course of immunotherapy.
- Cardiology: Acute Event Prediction: Beyond heart failure, AI for cardiology treatment personalization excels at predicting acute events such as stroke or myocardial infarction by detecting subtle, continuous changes in EHR and physiological data. AI-enabled risk stratification enables preemptive management, drastically reducing mortality and hospitalization costs.
- Infection Control (Sepsis): AI models for sepsis prediction, a leading cause of hospital mortality and high LOS, provide an average ROI of 4:1 in hospitals by accelerating diagnosis by several hours, enabling rapid antibiotic administration, and reducing ICU time. This is a crucial application of AI for optimizing hospital treatment.
- Rare Disease and Genomics: AI for rare disease treatment personalization integrates symptom profiles with advanced AI to discover predictive biomarkers, shortening the diagnostic window. In a pediatric setting, this can save up to $2 million over a child's lifetime by avoiding unnecessary specialist visits and procedures.
- Surgical Risk: AI for personalized patient care uses preoperative imaging and patient history to predict the individual risk of postoperative complications (e.g., wound infection, readmission). This enables preemptive nutritional or medical optimization, reducing surgical complications by 10-15%.
The Pharmacology Advantage: AI for Personalized Drug Development
In life sciences, AI for personalized drug development is the ultimate risk-mitigation strategy, maximizing the value of every molecule and ensuring its effectiveness.

- De Novo Drug Design: Generative AI is used for de novo (from scratch) drug design, creating novel molecular structures optimized for specific targets. This drastically reduces the time and cost associated with synthesizing and screening millions of compounds, accelerating the entire pipeline.
- Clinical Trial Site Optimization: AI for clinical trial optimization extends beyond patient selection to geographical site selection. AI models analyze demographic data, local disease prevalence, and the density of competing trials to recommend sites with the highest probability of rapid, successful patient enrollment.
- Optimizing Precision Dosing and Administration: AI for precision dosing uses pharmacokinetic and pharmacodynamic models to determine the exact optimal dose for an individual based on their metabolic profile and co-morbidities. This is critical for high-potency drugs, where the therapeutic window is narrow, and for maximizing the efficacy predicted by AI for drug response prediction.
- Post-Market Surveillance and Safety: AI continuously analyzes real-world data and social media for early signals of adverse drug events (ADEs) that might not have appeared in controlled trials. This proactive AI for therapy response prediction and monitoring reduces the risk of costly drug recalls and liability issues.
- Streamlining Regulatory Submissions: AI tools quickly aggregate and summarize the vast documentation required for regulatory submissions (FDA, EMA), making the process of obtaining AI for personalized drug development faster and less error-prone.
Strategic Implementation: From Pilot to Enterprise
Realizing the full ROI of AI for treatment personalization requires operationalizing the AI model through a well-governed, phased approach, supported by robust AI Development Services.
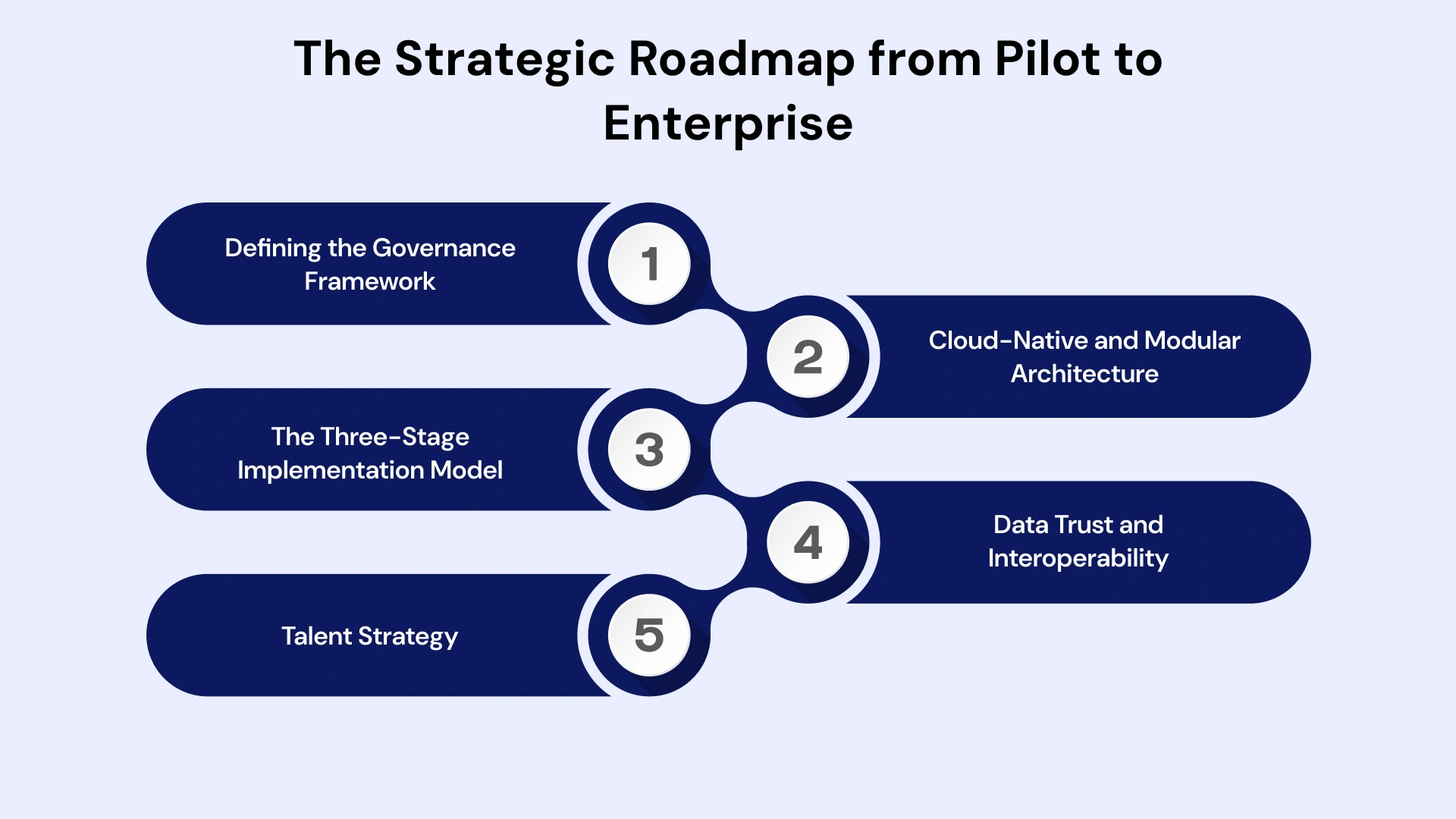
- Defining the Governance Framework: Before the first line of code, an organization must establish a cross-functional AI governance committee (clinical, legal, ethics, IT). This committee defines data access protocols, bias mitigation strategies, and the legal framework for using AI to generate personalized medicine outputs in clinical practice.
- Cloud-Native and Modular Architecture: Scaling AI requires a flexible cloud architecture (Azure, AWS, GCP). Solutions must be built using modular microservices so that a successful AI for personalized drug development model can easily share data pipelines with an AI for personalized patient management tool, reducing redundant infrastructure costs.
- The Three-Stage Implementation Model:
- Pilot and Validation (0-9 Months): Focus on one high-ROI use case. Engage AI Development Services and Clinical AI model development services for rapid prototyping and rigorous clinical validation using local real-world evidence for AI models.
- Scaling and Integration (9-24 Months): Leverage Healthcare Software Development Services to fully integrate the validated model into the EHR for enterprise use. This phase focuses on change management and training across all relevant clinical departments.
- Expansion and Optimization (24+ Months): Expand into new service lines (e.g., Cardiology to Pulmonology) and integrate AI to build personalized patient management tools for longitudinal patient engagement, maximizing the long-term ROI of AI in personalized treatment.
- Data Trust and Interoperability: Organizations must invest in data science infrastructure dedicated solely to maintaining data quality and standardization (e.g., FHIR-compliant data lakes). The inability of models to communicate or rely on inconsistent data is the number one cause of project failure.
- Talent Strategy: Organizations must decide whether to outsource AI Development Services or build and retain expensive in-house talent. A hybrid model, utilizing specialized AI healthcare consulting services for strategy and in-house staff for maintenance, often provides the optimal balance of cost and expertise.
Revolutionize Treatment Plans with VLink Software Development
The complexity of navigating data privacy (HIPAA/PHIPA), validating models for regulatory bodies, and integrating bleeding-edge AI into decades-old EHR infrastructure is the primary reason 42% of AI initiatives fail to meet ROI expectations.
VLink Software Development specializes in bridging this crucial gap between strategy and execution. We are your partner for AI Development Services and Healthcare Software Development Services, ensuring your investment in AI for treatment personalization delivers predictable, substantial returns.
Why VLink Maximizes Your AI ROI:
- HIPAA-Compliant AI Development: We build solutions with compliance and security embedded from day one, mitigating the multi-million-dollar risk of data breaches or regulatory fines. Our models are ready for SaMD classification.
- EHR Integration Mastery: We turn complex integration challenges into seamless workflows. Our dedicated team's expertise ensures that your AI for a clinical decision support system is operational within the existing clinical interface, driving high adoption and immediate impact.
- Full-Spectrum Clinical AI Expertise: From AI for oncology treatment planning to AI for patient recruitment and stratification, our clinical AI model development services deliver highly accurate, customized, and trustworthy predictive tools.
- Strategic Consulting: We offer AI healthcare consulting services to help you define the highest-ROI use cases, calculate Net Present Value (NPV), and build a defensible business case for your AI treatment personalization platform investment. We empower the affordability of AI-driven personalized medicine by providing flexible scaling models.
Conclusion: Securing the Future of Personalized Care
The Cost-Benefit Analysis of AI for Treatment Personalization is conclusive: the technology represents the single greatest opportunity for improving health outcomes while simultaneously tackling the crushing cost structures in healthcare. By generating over $3.20 for every dollar invested, the strategic adoption of artificial intelligence in personalized medicine is not a luxury—it is a competitive necessity.
The future belongs to the organizations—hospitals and pharma—that prioritize AI for treatment personalization, not just as a clinical tool, but as the core engine for operational efficiency and sustainable financial growth. The time to invest wisely, strategically, and with a focus on measurable ROI is now.
Ready to move beyond pilot projects and realize a sustained, measurable ROI from your AI investment? Partner with VLink to build the personalized treatment AI software that defines the future of your organization.








 Shivisha Patel
Shivisha Patel