The convergence of artificial intelligence and healthcare delivery is reshaping how organizations approach patient care, particularly in long-term care settings where operational complexity meets the demand for personalized attention.
The long-term care sector faces unprecedented challenges: an aging global population, persistent staffing shortages, escalating operational costs, and increasing regulatory complexity. Traditional management approaches struggle to address these multifaceted pressures while maintaining quality standards.
AI in long-term patient care represents not merely a technological upgrade but a fundamental reimagining of care delivery, operational workflows, and resource allocation strategies. From predictive analytics that anticipate patient deterioration to intelligent scheduling systems that optimize staff deployment, artificial intelligence services are becoming an indispensable component of modern elder care infrastructure.
For hospitals with extended care units, dedicated elder care centers, behavioral health providers, and mental health tech startups, understanding the strategic application of AI development services in long-term care has transitioned from a competitive advantage to an operational necessity.
This comprehensive exploration examines how organizations can leverage AI technology in long-term care operations to transform operations, improve clinical outcomes, and build sustainable care models that address both immediate operational challenges and the industry's long-term evolution.
Understanding the Current Landscape of Long-Term Care Operations
Long-term care facilities operate within a uniquely complex environment that distinguishes them from acute care settings. Unlike hospitals focused on episodic interventions, these facilities manage chronic conditions, progressive cognitive decline, and multifaceted care needs spanning months or years.
The operational reality involves coordinating medication management for residents with multiple prescriptions, documenting extensive care activities for regulatory compliance, managing dietary requirements, coordinating rehabilitation services, and maintaining appropriate staff-to-resident ratios across varying acuity levels.
Legacy long-term care EMR systems often exacerbate rather than alleviate these pressures, with fragmented interfaces, limited interoperability, and workflows that fail to reflect actual care-delivery patterns.
Quality Measurement and Complex Care Needs
Quality measurement in long-term care extends beyond clinical metrics to encompass resident satisfaction, family engagement, regulatory compliance, and financial sustainability. Facilities face scrutiny from multiple regulatory bodies, insurance providers, and quality reporting programs, each with distinct requirements and documentation standards.
The AI landscape in long-term patient care solutions has emerged to address these multidimensional challenges, offering integrated approaches spanning clinical decision support, operational optimization, and compliance management.
Behavioral health integration within long-term care adds additional layers of complexity. Residents with dementia, depression, anxiety, or other mental health conditions require specialized monitoring and intervention protocols. Traditional observation methods rely heavily on staff vigilance and documentation, creating potential gaps in early intervention opportunities.
Custom AI software development for elder care centers increasingly incorporates behavioral pattern recognition, enabling proactive identification of agitation, wandering risks, or mood deterioration before situations escalate.
Strategic AI Applications Transforming Long-Term Care Operations
The key to successful AI implementation is focusing on areas with the highest impact on safety, efficiency, and quality of life.
1. Predictive Analytics for Clinical Decision Support and Risk Management
Predictive analytics software for long-term care fundamentally alters the care paradigm by shifting from reactive responses to proactive interventions. These systems analyze historical patient data, vital sign trends, laboratory results, medication histories, and documented observations to identify patterns preceding adverse events.
A fall prevention system might integrate data from mobility assessments, medication lists, environmental factors, and previous incident reports to calculate individualized risk scores and recommend targeted interventions.
The implementation of AI in clinical practices, decision support for senior patients, has demonstrated a measurable impact across key quality indicators. Facilities deploying predictive models for sepsis identification report detection improvements of 12-18 hours, compared with traditional protocols, enabling antibiotic administration before full systemic involvement develops.
Similarly, pressure ulcer prediction algorithms analyze mobility limitations, nutritional status, skin condition assessments, and adherence to turning schedules to identify high-risk residents, facilitating enhanced prevention protocols before tissue damage occurs.
- AI for chronic patient management solutions extends beyond acute event prediction to optimize ongoing condition management. For residents with congestive heart failure, predictive models integrate weight, dietary and fluid sodium intake, activity levels, and medication adherence to identify early signs of decompensation.
- Hospital-based skilled nursing units benefit particularly from AI-driven readmission risk prediction. These models analyze discharge diagnoses, functional status assessments, medication complexity, social support factors, and post-acute care plans to identify patients at elevated readmission risk, directly impacting quality metrics and value-based payment performance.
- Building AI models for elderly fall detection is a specific, high-priority use case. Advanced models analyze gait changes over time, subtle posture shifts, and environmental data to predict falls before they occur, not just detect them after the fact.
The integration of AI in long-term patient care for behavioral health monitoring represents a particularly innovative application. Machine learning algorithms analyze speech patterns, movement characteristics, sleep patterns, and social interaction frequency to detect subtle changes that indicate mood deterioration, accelerated cognitive decline, or medication side effects.
2. Intelligent Automation for Workforce Optimization and Scheduling
Workforce management is a persistent operational challenge. Traditional long-term care scheduling software often fails to optimize for actual care requirements or staff capabilities.
AI automation for elder care operations transforms scheduling from an administrative burden to a strategic advantage. Modern systems ingest multiple data streams: resident acuity assessments, care plan requirements, staff credentials, availability, overtime budgets, and regulatory minimum ratios.
Machine learning algorithms then generate optimized schedules that balance clinical needs, cost constraints, and staff satisfaction. A facility might reduce overtime costs by 15-20% while improving staff schedule predictability. This is a core focus of innovation in long-term care scheduling software.
- AI for long-term care workflow optimization extends to real-time adjustment. When a staff member calls in sick, the system recalculates optimal coverage options, taking into account available on-call staff and cross-training certifications.
- An AI-powered long-term care system, integrated with time-and-attendance tracking, identifies workflow inefficiencies, duplicate documentation, and suboptimal task sequencing by analyzing actual task completion times.
- Long-term care management software with AI capabilities also addresses the challenge of matching staff expertise to resident needs. Beyond basic certification, systems consider staff experience with specific conditions (e.g., dementia care expertise) and interpersonal dynamics, improving care quality while reducing staff stress.
3. Remote Monitoring and Continuous Patient Surveillance Systems
The evolution of remote patient monitoring AI software has transformed continuous surveillance from resource-intensive observation to intelligent, automated alerting systems.
An AI apps for elderly patient monitoring typically integrate multiple data sources: wearable vital sign monitors, environmental sensors, bed/chair sensors, and, increasingly, computer vision systems for contactless monitoring.
The critical innovation lies in intelligent filtering and prioritization. AI algorithms distinguish routine movements from concerning patterns, and normal vital sign variations from clinically significant changes.
- AI for elderly health monitoring systems is particularly valuable for overnight surveillance. A resident attempting to get out of bed unassisted triggers immediate staff notification with location and context.
- Hospitals with skilled nursing units utilize AI solutions for nursing homes to extend ICU-level monitoring capabilities to step-down care environments. Algorithms identify subtle pattern changes hours before cardiac events or respiratory distress, well before traditional alerts.
- AI-driven care coordination applications integrate monitoring data with care planning. When a resident exhibits declining mobility, the system automatically schedules a physical therapy reassessment, updates fall risk protocols, and notifies relevant care team members.
Operational Efficiency Improvements Through AI Integration
Beyond direct patient care, AI dramatically improves the efficiency and compliance of facility operations.
1. Documentation Automation and Administrative Burden Reduction
Clinical documentation is a significant burden, consuming up to 35% of nursing time. Artificial intelligence development services company providers have focused on natural language processing (NLP) and ambient documentation technologies.
Modern AI approaches leverage speech recognition and contextual understanding to transform conversational care delivery into compliant documentation. A nurse describing wound care can have the system automatically capture wound dimensions, treatment provided, and the resident's response, thereby populating assessment forms. This ambient documentation approach can reduce documentation time by 40-50%.
- Healthcare software development tailored to long-term care incorporates predictive text, innovative forms, and contextual suggestions that streamline recurring entries, requiring only confirmation rather than complete manual entry.
- Gen AI service capabilities enable automatic compliance checking, identifying missing required assessments or documentation gaps that might trigger survey deficiencies.
- AI agents' pricing models for documentation assistance vary, but the return on investment (ROI) is significant, driven by increased staff productivity and reduced compliance risk.
2. Supply Chain Optimization and Resource Management
AI technology applied to long-term care operations for supply chain management creates significant cost-reduction opportunities.
Predictive inventory management systems analyze consumption patterns, resident census trends, and supplier lead times. Facilities implementing AI-driven inventory management report 15-25% reductions in supply costs through waste reduction and improved vendor negotiation.
- AI tools for senior care software companies developing supply chain solutions increasingly incorporate predictive maintenance. By analyzing equipment utilization and sensor data from critical assets, AI predicts failure risk and optimizes preventive maintenance scheduling.
- Custom AI solutions for senior care centers manage pharmaceuticals by tracking utilization, identifying prescribing patterns, detecting potential drug interactions, and suggesting generic substitutions that reduce pharmacy costs while maintaining clinical effectiveness.
3. Quality Improvement and Regulatory Compliance Enhancement
AI tools for improving elder care quality consolidate multidimensional data streams (clinical outcomes, resident satisfaction, regulatory compliance) into integrated dashboards that identify opportunities for improvement. This is a crucial element of AI app development for long-term care facilities.
- The benefits of AI in long-term patient care apps for quality management include automated calculation of quality indicators and trend identification. A facility might receive early notification that infection rates are trending upward, enabling immediate process review.
- Regulatory survey preparation is streamlined. AI-powered long-term care system development incorporates continuous compliance monitoring that simulates survey processes, reviews documentation for common deficiency patterns, and generates corrective action recommendations.
Implementation Strategy: AI Technology Stack and Development
To successfully implement these solutions, organizations must understand the underlying technology and approach.
The AI Technology Stack for Long-Term Care Apps
A robust AI technology stack for long-term care apps typically involves several layers, ensuring data is collected, processed, analyzed, and delivered as actionable insights.
Layer | Components & Function |
Data Acquisition | Sensors (wearables, environmental), IoMT devices, EMR/EHR systems (Long Term Care EMR Software) |
Data Processing | Cloud/Edge Computing (for real-time analysis), Data Lakes, Data Warehouses |
Model Development | Machine Learning Frameworks (TensorFlow, PyTorch), Custom AI Solutions for Senior Care Centers algorithms (NLP, Computer Vision, Predictive Models) |
Application Layer | Intelligent elder care app development, APIs for integration, User Interface/Dashboards |
Security & Compliance | Encryption, HIPAA-compliant cloud services, Blockchain (for data integrity) |
AI in Long-Term Care Software Development
Working with an AI patient monitoring app development company or an artificial intelligence development services company requires a strategic approach:
- Custom AI software for elder care centers is often necessary because off-the-shelf models may not be trained on the specific, complex data of long-term care residents (e.g., polypharmacy, complex chronic conditions).
- AI in long-term care software development requires specialized expertise in clinical data, privacy, and regulatory adherence.
- AI integration for elder care management systems is critical. The AI system must seamlessly exchange data with the core EMR/EHR to ensure staff use a single, unified source of truth.
How to Build an AI Platform for Long-Term Care Facilities
Building a successful AI platform for long-term care facilities is a multi-stage process that focuses on integrating technology with clinical reality:
1. Define the Problem & Data Strategy: Start with a clear problem (e.g., "high fall rate" or "inefficient scheduling"). Identify all necessary data sources (EMR, sensor data, staffing records). The platform must be built on a foundation of high-quality, normalized data.
2. Select the AI Technology Stack: Choose the appropriate cloud environment and machine learning tools. Focus on tools that offer strong security and simple AI integration for elder care management systems.
3. Develop and Train Models: Work with an artificial intelligence development services company to train a model specific to your resident population and clinical goals. This requires a robust, iterative process of model testing and validation.
4. Integration and Workflow Embedding: This is the most critical stage. The AI platform must be integrated directly into the care team's existing workflows (e.g., via the best AI features in long-term care software within the EMR or on staff mobile devices).
5. Pilot, Measure, and Scale: Begin with a controlled pilot, rigorously measure the impact on key metrics (e.g., reduced overtime, earlier detection), and then scale the successful deployment across the organization.
AI Use Cases in Long-Term Care Software Development
The specific AI use cases in long-term care software development are centered around high-risk, high-volume tasks:
Use Case Category | Specific AI Application | Value Proposition |
Clinical Safety | Building AI models for elderly fall detection | Reduces patient injury, lower litigation risk. |
Medication Management | Drug-drug interaction flagging, dosage optimization | Reduces adverse drug events and related hospitalizations. |
Staffing & Operations | Intelligent Staff Scheduling and Coverage Recalculation | Reduces staff burnout, cuts overtime costs. |
Behavioral Health | Sentiment analysis of care notes, agitation pattern recognition | Proactive intervention, reduced the need for chemical restraints. |
Quality/Compliance | Automated Quality Measure Calculation & Deficiency Auditing | Improves regulatory survey readiness and performance metrics. |
AI in Long Term Care: Cost, Benefits, and Ethical Considerations
A comprehensive plan must address the ROI and the responsibility of deploying AI in care settings.
Benefits of AI in Long-Term Patient Care Apps
The adoption of AI app development for long-term care facilities yields clear returns across multiple dimensions:
- Enhanced Clinical Outcomes: Earlier detection of sepsis, UTIs, and falls, leading to better patient safety and reduced readmission rates.
- Improved Efficiency: Reduced documentation time for nurses, optimized schedules, and lower supply costs.
- Financial Sustainability: Lower operational costs and improved performance in value-based care models.
- Staff Retention: Reduced administrative burden and less reliance on staff for constant, manual monitoring.
Cost to Develop AI Long-Term Care Software
The cost to develop AI long-term care software is a significant investment that requires careful budgeting.
- Licensing vs. Custom Development: Licensing commercial, off-the-shelf solutions (e.g., AI solutions for nursing homes) is faster and cheaper in the short term. Full-custom AI solutions for senior care centers require a higher upfront investment in an artificial intelligence development services company, but offer maximum tailoring to existing workflows.
- Integration Costs: The complexity of integrating the new AI system with legacy long-term care EMR software is often a primary cost driver. Robust AI integration for elder care management systems requires specialized APIs and development hours.
- Data and Model Training: Significant costs are incurred for data cleaning, normalization, and the computational power required to train complex machine learning models.
Ethical Considerations and Human-Centered Care Balance
The successful adoption of intelligent elder care app development relies on balancing technological capability with ethical responsibility.
- Autonomy and Consent: Organizations must establish clear policies for notifying residents about AI-enabled monitoring, especially given the prevalence of cognitive impairment. Consent must be specific and understandable.
- Algorithmic Bias: Training data may not reflect the demographic diversity of long-term care residents, potentially leading to systems that are less accurate for minority populations. Organizations must demand that vendors demonstrate ongoing bias monitoring and performance assessment across demographic groups.
- Transparency and Trust: Staff must retain clinical judgment as the primary driver, viewing AI as clinical decision support for senior patients rather than a decision replacement. Staff need to know how the system works and when their judgment should override the system's suggestion.
Future of AI in Long-Term Care
The future of AI in long-term care will see AI move from pilots to a core layer that supports care delivery, staffing, and reimbursement, helping providers stay sustainable as the aging population grows and staffing shortages intensify.
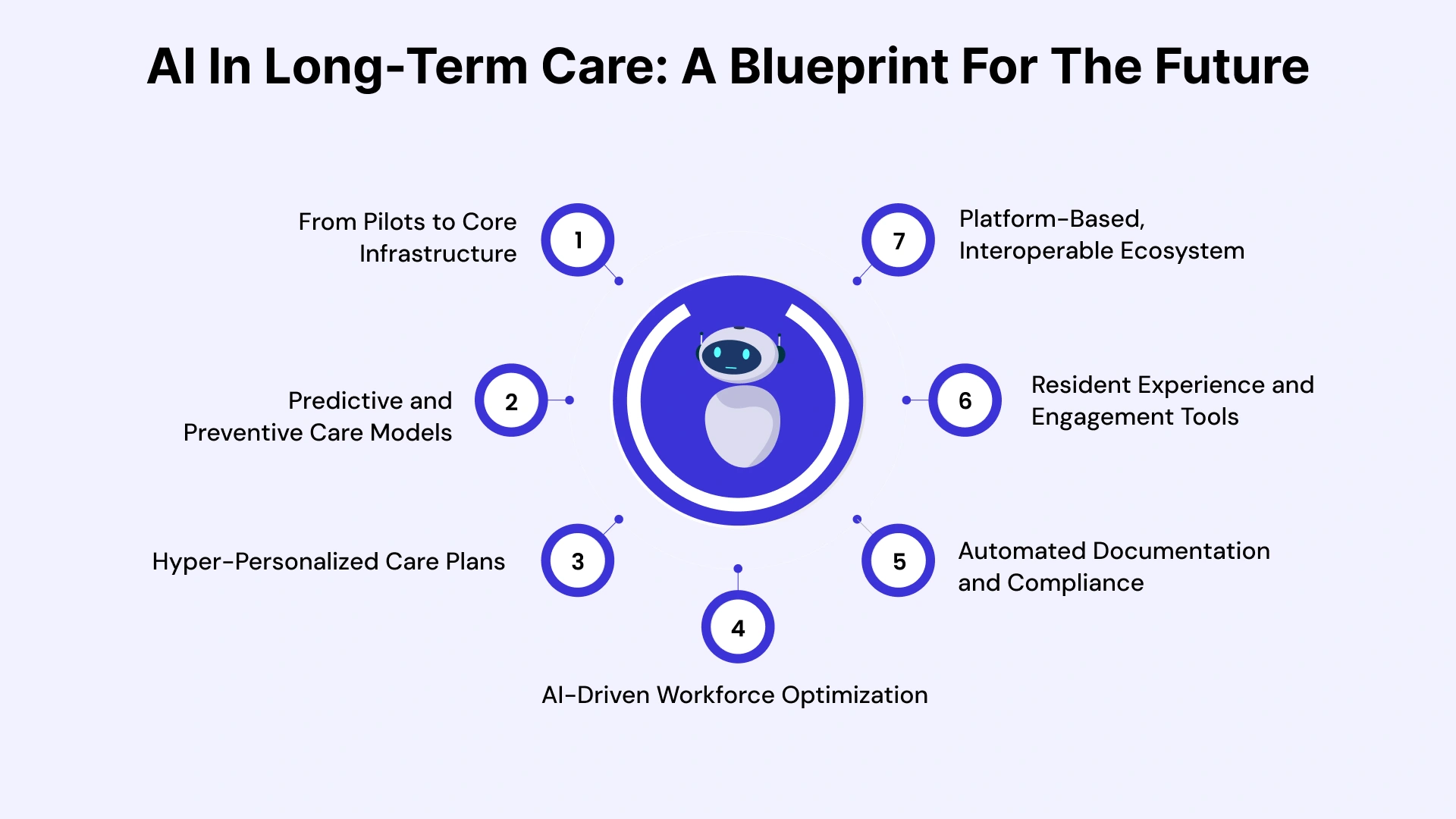
- From Pilots to Core Infrastructure: AI will evolve from isolated experiments into an integrated “nervous system” that connects EHRs, sensors, and workflow tools across long-term care facilities, standardizing data and insights in a single place.
- Predictive and Preventive Care Models: Advanced analytics will continuously monitor resident health indicators to predict falls, infections, and deterioration days in advance, enabling early interventions rather than crisis-driven care.
- Hyper-Personalized Care Plans: AI will help care teams build dynamic, individualized care plans that adjust in real time based on residents’ clinical data, behavior patterns, and response to treatment, improving outcomes and satisfaction.
- AI-Driven Workforce Optimization: Intelligent staffing and scheduling tools will match staffing levels to resident acuity and forecast workload, reducing burnout while ensuring the right skills are available at the right time.
- Automated Documentation and Compliance: Natural language and automation tools will capture notes, populate forms, and support quality and regulatory reporting, giving clinicians more time for direct resident interaction rather than paperwork.
- Resident Experience and Engagement Tools: AI-powered virtual assistants, social robots, and smart rooms will support companionship, cognitive stimulation, and adherence to care routines, reshaping how residents experience independence and connection.
- Platform-Based, Interoperable Ecosystems: The competitive edge will shift to providers that build interoperable AI platforms, linking EMR data, IoT devices, and analytics under strong governance to drive measurable gains in quality ratings, occupancy, and financial performance.
Choose VLink AI Expertise in Long-Term Care
As healthcare organizations navigate the complex landscape of AI long-term care software development, partnering with experienced development teams becomes crucial for successful implementation and sustained value delivery.
VLink brings specialized expertise in Healthcare Software Development that addresses the unique requirements of long-term care environments, combining deep clinical domain knowledge with cutting-edge artificial intelligence service capabilities. Our approach to custom AI software for elder care centers begins with a comprehensive discovery that maps your specific operational challenges, existing technology infrastructure, regulatory requirements, and strategic objectives.
Whether you're a multi-facility senior care operator seeking enterprise-wide predictive analytics, a hospital expanding skilled nursing capabilities, or a behavioral health startup building AI in long-term patient care solutions, VLink's flexible engagement models support your specific needs.
Full-Cycle AI Implementation and Support
VLink's artificial intelligence development services capabilities span the full AI implementation lifecycle, ensuring seamless integration and adoption:
- Data Science & Engineering: We develop robust predictive analytics software for long-term care, trained on healthcare-specific datasets, and build scalable architectures that integrate seamlessly with existing long-term care EMR systems.
- UX & Implementation: Our skilled designers create intuitive interfaces, while our specialists manage change management, training, and go-live support, driving adoption and value realization.
Compliance, Security, and Partnership
Security, compliance, and reliability are non-negotiable. VLink maintains SOC 2 Type II certification and HIPAA compliance frameworks. Our AI technology stack for long-term care apps incorporates industry-leading security protocols, redundancy, and disaster recovery capabilities for continuous availability.
Recognizing the constraints on the cost of developing long-term care AI software, VLink offers flexible engagement models (fixed-price, time-and-materials, dedicated teams) with transparent estimation processes. Post-implementation support provides comprehensive packages for system monitoring, optimization, and regulatory updates, ensuring your AI solutions continue to deliver maximum value.
Conclusion: Embracing AI-Driven Transformation in Long-Term Care
The transformation of long-term care through artificial intelligence is an operational imperative for sustainable, high-quality care delivery. The convergence of demographic pressures, workforce constraints, and cost demands creates an environment where traditional approaches are insufficient. AI in long-term care offers practical, measurable solutions.
The strategic applications we explored—predictive clinical analytics, intelligent workforce optimization, and continuous monitoring—demonstrate AI's capacity to enable fundamentally different care models that successfully balance personalization, safety, and staff sustainability.
Successful AI adoption requires thoughtful implementation that prioritizes human-centered care, ethical considerations, and stakeholder engagement. Facilities achieving the most outstanding benefit view technology as an enabler of the human connections and compassionate care that define excellence.
Organizations that navigate this journey thoughtfully will thrive through enhanced quality, improved efficiency, and differentiated care models. The future of long-term care will increasingly feature AI as foundational infrastructure.
Ready to Transform Your Long-Term Care Operations with AI? VLink's specialized healthcare development team has the expertise and commitment to translate AI potential into operational reality. Contact us today to schedule a consultation with our long-term care AI specialists.








 Shivisha Patel
Shivisha Patel